The United States Medical system is a complex and multifaceted network that plays a critical role in the health and well-being of its citizens. According to Dr. Alice Chen, a prominent expert in health policy, “Understanding how the United States Medical system operates is essential for navigating the challenges of healthcare access and quality.” This statement underscores the importance of comprehending the intricate components that make up the system, including hospitals, insurance providers, and regulatory bodies.
The United States Medical framework encompasses a broad spectrum of services and innovations, all designed to meet the diverse health needs of the population. From primary care practitioners to specialized medical institutions, each segment contributes to a holistic approach toward health. Moreover, the interplay between public and private sectors within this system shapes the experiences of patients seeking care, often impacting their accessibility to necessary treatments and services.
As we delve into the workings of the United States Medical system, it is crucial to shed light on both its strengths and weaknesses. Analyzing factors such as healthcare funding, patient outcomes, and policy decisions will provide a clearer picture of how the system operates and its effects on everyday lives. Understanding this dynamic landscape is not just valuable for experts, but also imperative for anyone looking to navigate their healthcare journey effectively.

The United States medical system is complex and multifaceted, encompassing various elements from private practices to major healthcare institutions. At its core, the structure is divided into public and private sectors, where both play significant roles in how care is delivered. According to the American Hospital Association, there are over 6,200 hospitals in the U.S., which operate under different regulatory frameworks and funding models. Approximately 65% of hospitals are non-profit, significantly affecting how resources are allocated and patient care is administered.
In navigating this system, understanding health insurance is paramount. The Centers for Medicare & Medicaid Services reports that nearly 91% of Americans are covered by some form of health insurance, with private insurance making up a substantial portion of that coverage. This can impact access to various services and the overall quality of care patients receive. The structure often leads to variations in standards and practices across states and regions, which can pose challenges for patients seeking consistent care.
Tip: When selecting healthcare options, consider reviewing your insurance plan's coverage and network of providers. This ensures that your healthcare choices align with what is financially feasible and accessible. Additionally, maintaining up-to-date knowledge of policy changes can help individuals navigate potential shifts in their health care accessibility.
This bar chart represents the healthcare expenditure distribution across various sectors in the United States for the year 2021. The expenditure is measured in billion USD, showcasing where most of the healthcare funding is allocated.
In the U.S. healthcare ecosystem, three key players—providers, payors, and patients—interact in complex ways that shape the overall system. Providers refer to the individuals and institutions delivering healthcare services. This group includes physicians, hospitals, clinics, and allied health professionals. Their primary role is to diagnose, treat, and manage patients’ health conditions. The quality of care offered by providers can significantly influence patient outcomes, reflecting the importance of accessibility and standards in healthcare.
Payors, on the other hand, encompass insurance companies, government programs, and other entities that finance healthcare services. They determine how much providers are reimbursed for the services they provide and play a crucial role in determining patients' financial responsibilities like copayments and deductibles. The relationship between payors and providers often dictates the scope of services available to patients and can affect the overall cost of care. In turn, patients are the recipients of healthcare services, navigating this intricate system to seek treatment, manage their health, and make financial decisions about their care. Their engagement and awareness of benefits, costs, and available options are vital for optimizing their healthcare experience.

In the United States, health insurance is categorized into two primary models: public coverage and private coverage. Public health insurance is primarily funded and managed by the government, providing coverage to specific populations. This includes programs such as Medicare, which serves the elderly and certain disabled individuals, and Medicaid, aimed at low-income families and individuals. These programs are essential in ensuring vulnerable groups have access to necessary medical services, although they often come with specific eligibility criteria and limitations in certain areas of care.
On the other hand, private health insurance is typically provided through employers or can be purchased individually. This model offers more flexibility in choosing healthcare providers and often includes a wider range of services. However, private insurance plans can vary significantly in terms of cost, coverage options, and out-of-pocket expenses. Because private coverage is more market-driven, it can lead to disparities in access to healthcare based on an individual's financial means or employment situation. As a result, while both public and private models play vital roles in the U.S. healthcare landscape, they contribute to differing experiences and outcomes in healthcare access and affordability.
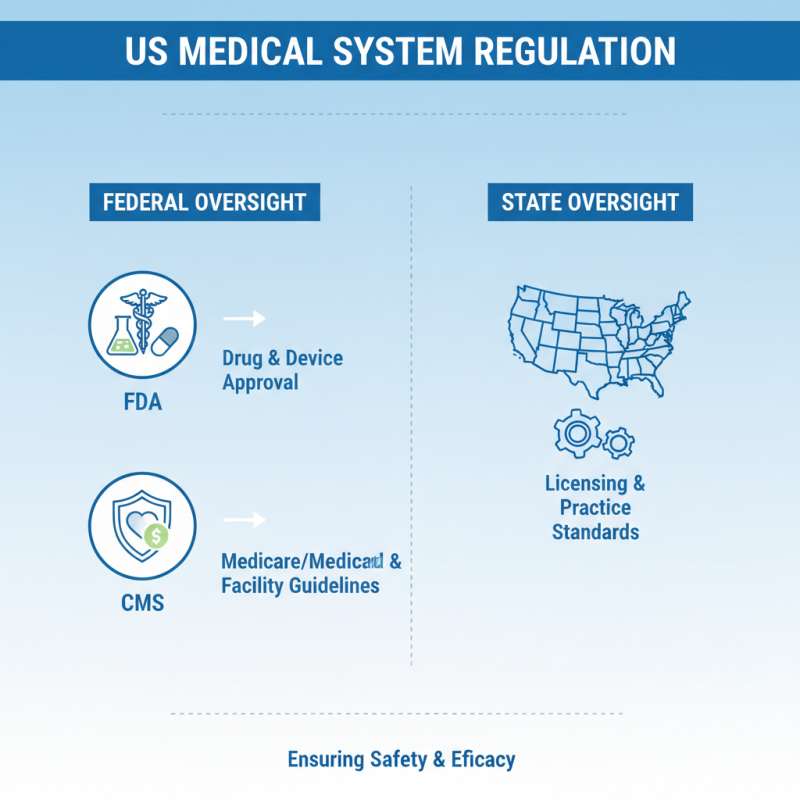
The regulatory framework governing the United States medical system is complex, involving both federal and state oversight to ensure public safety and efficacy in healthcare delivery. At the federal level, agencies such as the Food and Drug Administration (FDA) and the Centers for Medicare & Medicaid Services (CMS) play critical roles. The FDA is primarily responsible for the approval of drugs and medical devices, ensuring that they meet rigorous safety and efficacy standards before they can be marketed. Meanwhile, CMS oversees the nation's public health insurance programs, establishing guidelines that facilities must follow to receive federal funds.
State governments also have significant authority in regulating healthcare within their jurisdictions. They enforce medical practice acts that determine who can practice medicine and under what conditions. Additionally, state health departments often handle the licensing and regulation of hospitals, clinics, and healthcare professionals, adapting federal guidelines to local needs. This dual structure of regulation allows for a more tailored approach to healthcare delivery, though it can create challenges in consistency and compliance across state lines. Ultimately, navigating this intricate web of regulations is essential for providers as they seek to deliver safe and effective patient care.
The U.S. healthcare delivery system is currently grappling with several significant trends and challenges. One of the most pressing issues is the increasing cost of healthcare, which has been a persistent concern for both consumers and policymakers. The rise in prices has outpaced inflation, leading to greater financial strain on households and creating barriers to access for essential services. Many individuals find themselves either uninsured or underinsured, making it difficult to seek timely medical attention, which can lead to worse health outcomes.
Another critical trend involves the integration of technology in healthcare delivery. While advancements such as telemedicine and electronic health records promise to enhance efficiency and accessibility, they also raise questions about privacy, data security, and equity. Vulnerable populations may struggle to benefit from these technological innovations due to a lack of access to reliable internet and digital literacy. Additionally, the ongoing evolution of healthcare policies, particularly in the wake of the COVID-19 pandemic, reflects a growing recognition of the need for adaptable and resilient healthcare systems that can respond effectively to public health crises.
As the U.S. healthcare system continues to evolve, addressing these challenges requires collaborative efforts from government, healthcare providers, and communities. It is essential to develop innovative models that prioritize quality care and equitable access while managing costs. Ensuring that all Americans can obtain the care they need, when they need it, will be crucial in creating a more sustainable and effective healthcare delivery system.